What You Need to Know About Colon Polyps
What Are Polyps?
A polyp is an abnormal growth of tissue on the inner lining of the colon or the rectum. They can occur in other locations in the gastrointestinal tract but are most common in the colon. People can have several polyps scattered in different parts of their colon.
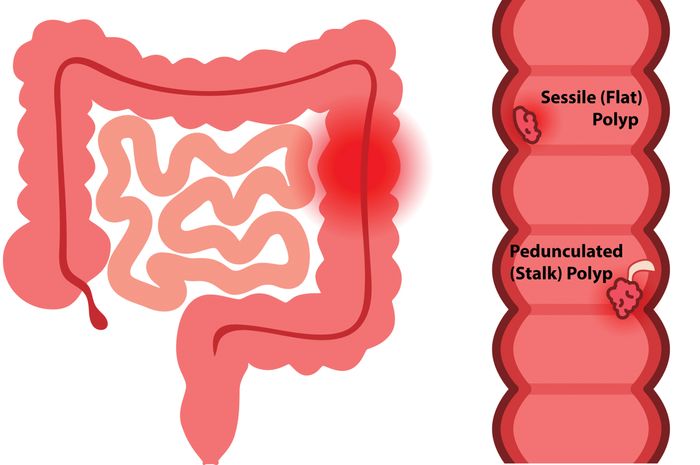
Polyps can vary in size from less than a quarter of an inch to several inches in diameter. They look like bumps growing from the inside lining of the colon protruding into the lumen. They sometimes grow on a “stalk” and look like mushrooms. Some polyps can be flat.
Colon and rectal polyps occur in about 25 percent of men and women ages 50 and older. Recent studies revealed an increase in the number of people, younger than 50, who develop polyps, when compared with the past. To address this trend the American Cancer Society is now recommending that screenings begin at age 45. Some polyps can contain cancer, although the vast majority of polyps do not. Larger polyps are more likely to become cancerous than smaller ones.
What Causes Polyps?
Medical experts are not sure what causes colon polyps. Anyone can develop colon or rectal polyps, but research suggests that certain factors, such as age and family history, can increase the chances of developing colon polyps.
People with the following factors are at a higher risk, according to the American Cancer Society:
- Age 45 and older
- A family history of polyps or colon cancer
- Rare inherited genes that make people more likely to develop polyps
- An inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease
- A high-fat, low-fiber diet
- Tobacco and alcohol use
- A habit of little or no exercise
- Obesity
According to research from the American Cancer Society (ACS), since the mid-1990s, the rate of colon cancer in adults younger than 50 has seen a steep increase. Because of this change, ACS is now recommending that people 45 and older get colonoscopy screenings.
How Are Polyps Detected?
A colonoscopy is considered the “gold standard” for colon cancer screening. Polyps detected by other screening tests require a colonoscopy for removal. Polyps can be detected and safely removed during a colonoscopy, preventing them from turning into cancer. Large polyps may require more than one treatment, and in some patients surgery could be required for complete removal.
Studies show that regular screening with colonoscopy and removal of polyps reduces your risk of developing colorectal cancer by up to 70 percent.
What Do Polyps Look Like?
There are two types of polyp shapes: the sessile or flat polyp, and the pedunculated polyp, which has a stalk. Sessile polyps lie flat against the surface of the colon’s lining. Because they do not protrude from the colon wall, they are harder to detect during a colon cancer screening. Pendunculated polyps are mushroom-like tissue growths that attach to surface of the colon’s mucous membrane by a long, thin stalk.
How Are Polyps Removed?
Almost all precancerous polyps that are discovered during a screening colonoscopy can be completely removed during the procedure. Removing them is called a polyp resection or polypectomy. Various techniques are used to remove polyps, including using a wire loop or biopsy forceps, or sometimes using electric current.
Because the lining of the colon is not as sensitive to cutting or burning, polyp resection usually does not cause any discomfort. Polyp removal is a routine procedure. Complications are rare, but may include bleeding or a perforation (a hole or tear) of the colon.
Any polyps that are removed during your colonoscopy will be sent to a lab for analysis. It usually takes two to three business days before the biopsy results are available. We will provide you with a report indicating the type of polyp that was removed and if any further action needs to be taken.
How Often Must I Have a Screening Colonoscopy?
The presence of a polyp only means that you are at risk for colon cancer. Colon cancer is the third most common cancer in the United States and, with regular screening colonoscopies, one of the most preventable and curable.
The timing of your next colonoscopy depends on several factors, including the type, number and size of polyps removed. Based on these and other factors, like family history of colon cancer, your gastroenterologist will decide when your next colonoscopy is necessary.
If your doctor recommends a follow-up colonoscopy, PA GI will send out a reminder notice, so that you can stay on schedule with your preventive care.
Because polyps and colon cancer run in families, it is extremely important that you notify your parents, children and siblings if you have a polyp or cancer discovered during your colonoscopy. Your family members should speak with their doctors about having a screening colonoscopy.
